if you have a sleep disorder, we can help.
At Allergy and Pulmonary, our physicians are committed to diagnosing and treating patients with the broad spectrum of Sleep Disorders. Many Americans don’t realize they have sleep disorders and continue their day to day lives without ever being diagnosed.
The reality is that sleep disorders have crucial effects on your life. Lack of sleep creates accidents on the road and in the workplace. It affects your cognitive process and your ability to think and learn effectively. Loss of sleep decreases your sex drive and can lead to high blood pressure, heart disease, heart attack, stroke, and diabetes.
We provide evaluation, diagnostic testing and treatment of a variety of common symptoms such as snoring, excessive daytime sleepiness, insomnia and fatigue. We offer diagnosis and treatment of a variety of sleep disorders including, but not limited to:
- Snoring Insomnia and Excessive Sleepiness
- Obstructive Sleep Apnea
- Narcolepsy
- Parasomnias and Abnormal Sleep Behaviors
- Periodic Limb Movement Disorder
- Restless Legs Syndrome
- Circadian Rhythm Disorders
AMERICAN THORACIC SOCIETY – CPAP for adults with obstructive sleep apnea

OSA (also called sleep apnea) is a common disorder in which people stop breathing while they are asleep. Studies suggest at least 10% of the US population has OSA. In OSA, the back of the throat collapses multiple times off and on throughout the night causing the airflow into the lungs to be cut off.
OSA patients wake up often throughout the night (although they may not remember doing so) and thus can be very tired during the daytime. In addition, each stoppage in breathing can lead to falls in oxygen level and a stress release of adrenaline, both of which can contribute to high blood pressure and put a strain on the heart. Left untreated, this situation can lead to serious health risk. Studies show that treatment of sleep apnea can make people feel better and reduce the risk of serious medical complications.
What is CPAP?
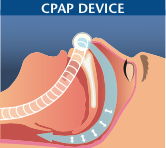
CPAP stands for continuous positive airway pressure. CPAP is being used by millions of people in the US every night. Your provider can get you a CPAP machine by writing a prescription with the machine provided either through a durable medical equipment (DME) compa- ny or sometimes via the provider’s office. CPAP is delivered using a mask that covers the nose (or sometimes both the nose and mouth). CPAP works by blowing air into the nose and throat. This blowing of air causes a positive pressure to hold the upper airway (back of the throat) open during sleep. When the upper airway is open, airflow can pass to the lungs undisturbed. A person using CPAP will sleep more soundly without snoring or arousals. CPAP almost always can help sleep apnea if people tolerate it, but some patients find it uncomfort- able. At times this discomfort can be reduced by use of a different mask and/or adjusting the settings of the CPAP. People with sleep apnea need to use CPAP every time they sleep to maximize benefits.
What causes OSA?
OSA is thought to be a disease where the back of the throat is small- er which can then cause it to collapse easily. In addition, the upper airway muscles, which hold the throat open, do not work properly in people with OSA. Also, the brain tells us when to breathe and sometimes the breathing pattern during sleep can be abnormal in OSA. Recent studies suggest that not all people with OSA have the disease for the same reason. Health care providers and researchers are continuing to figure out ways to personalize treatments to target to the underlying cause(s) rather than just take a ‘one size fits all approach’ to all people with sleep apnea.
How do I know if I have OSA?
OSA patients often complain of snoring and daytime sleepiness, but sometimes symptoms are not obvious. Subtle forms of OSA are quite common and people who have certain medical conditions can be at high risk. People at high risk of sleep apnea include those who are male, elderly, women after menopause, or who are obese. People with diabetes, sickle cell disease, and those with heart or lung disease (such as asthma, emphysema or COPD) may be at special risk. If you think you might have sleep apnea, you should talk to your health care provider. A simple home sleep test often can usually be done to make a diagnosis, although in-laboratory sleep testing (polysomnography) can be helpful in select cases. The sleep apnea diagnosis is usually made by a combination of history and physical examination plus some form of sleep testing. For more information, see ATS Patient Information Series piece “Sleep Studies”.
Will my OSA ever go away?
In general, OSA is considered a lifelong condition, although there are a few exceptions in which OSA can improve or go away. Obesity isa major risk factor for OSA and weight loss has been shown to lead to improvement in OSA. Major weight loss can be very difficult to achieve through diet and exercise although some people are success- ful. At times, a patient may need help from a health care provider to help lose weight safely. Stomach stapling (bariatric surgery) can be highly effective for losing weight, although as with any surgery, complications can occasionally occur. The other situation in which apnea can resolve is in people with large tonsils that are blocking airflow in the throat. Removal of tonsils, particularly in children, has been shown to improve OSA. However, removal of tonsils is typically not sufficient to treat OSA in adults.
Why should I wear CPAP at night?
There are three major benefits from using CPAP with sleep:
- Snoring is often annoying to the bed partner, such that many people with sleep apnea use CPAP to keep their partner happy. Some people think snoring is funny or a nuisance, but it can have a big impact on quality of life if it interferes with intimacy or disrupts the sleep of the bed partner. Some studies suggest that snoring may have effects on the blood vessels in the neck which can affect blood flow to the brain; however, the risks of snoring itself (without sleep apnea) beyond the noise it produces remain unclear.
- CPAP can improve symptoms. Many people feel better after wearing nightly CPAP. Research trials have shown improved daytime sleepiness, quality of life, and reduced risk of car accidents.
- CPAP can improve cardiac and diabetes risk. CPAP has been shown in research trials to improve high blood pressure and likely reduces the risk of heart attack and other serious medical conditions. Large scale research trials are still in process to examine the long-term benefits of CPAP.
Can OSA kill me?
Some people hear about stoppages in breathing and get very wor- ried that sleep apnea may kill them during sleep. For the most part, people with OSA wake up from sleep rather than allowing stoppages in breathing to go on for a long time. Some long term studies have shown that if OSA goes on for years without treatment that the risk of death may increase slightly. However, OSA is not considered a rapidly fatal disease, but rather a disease that can cause long term health problems without treatment.
What happens if I can’t tolerate CPAP therapy?
CPAP therapy can provide major benefits for some patients but it is not for everyone. Most sleep experts will recommend further at- tempts of a different type of positive airway pressure therapy for patients who don’t like CPAP. A variety of masks and pressure delivery approaches are available so patients are encouraged to try various devices before giving up. Education and support can also be helpful in getting people used to using the CPAP machine. Sometimes psychologists or respiratory therapists can be helpful in getting you get used to the equipment and being able to sleep with the equipment on. CPAP can be uncomfortable when you are not used to it, but is not invasive, so many patients do well if they stick with it over time.
Are there alternative therapies for OSA?
There are alternative treatments for OSA beyond CPAP that can be helpful for some people (For more information see ATS Patient Information Series piece “Alternative Therapies” at www.thoracic.org/patients).
- Oral appliances are made by dentists and can be useful to pull the jaw forward and help to prevent collapse at the back of the throat. Some people prefer oral appliances to CPAP although in most studies CPAP is more effective at controlling OSA.
- Surgery can be performed on the upper airway, but the improvements in OSA vary from person to person. Some studies show elimination of OSA in highly selected patients who undergo major operations on the throat, whereas other patients have no major change in their OSA particularly following minor surgical procedures. One type of surgery for sleep apnea is the uvulopalatopharyngoplasty (UPPP) which involves cutting the soft palate at the back of the throat. Not everyone will benefit from this surgery. Researchers are still trying to figure out which patients respond best to this procedure.
- Hypoglossal nerve stimulation (HGNS) uses a pacemaker-like stimulator device that a surgeon places in the neck and use electricity to activate the muscles in the tongue to hold the airway open. HGNS recently received approval by the Food and Drug Administration (FDA) and is being used increasingly in the past year.
- There are some devices that can be purchased at the drug store such as special pillows and nasal strips, but unfortunately most of these treatments do not work and/or there has not been enough research to determine if these are helpful.
What is expected in the future for sleep apnea?
Improvements are expected both on the diagnosis and treatment of OSA. Home sleep study testing is becoming common and research continues for getting information about breathing during sleep through smartphones or electronic wrist devices. The goal of testing will be not only to provide a diagnosis (does the person have sleep apnea or not), but also to define high risk patients (e.g. who needs CPAP therapy right away and who is likely to benefit from treatment). It is also hoped new tests will help better define the underlying causes of OSA (why a given patient has sleep apnea or not). Nasal CPAP will continue to be the main treatment for OSA for some time, but efforts are ongoing to develop new devices to hold the airway open or pharmacotherapy (medicines) to eliminate apnea. Health care providers will consider what is the best approach for each person.
Why are there so many devices that sound like CPAP? Are they all the same?
CPAP is continuous positive airway pressure, whereas APAP is au- tomated positive airway pressure and BiPAP is a brand name which describes bi-level positive airway pressure. When talking about these therapies in general some people just use the term PAP (positive air- way pressure) or use the term CPAP somewhat loosely to include all of the various therapies. CPAP is delivered at a fixed pressure which your provider can determine based on either in-laboratory titration or from an APAP device. APAP varies the pressure to keep the airway open with each company having a slightly different method to determine the ideal pressure. APAP devices are used commonly after home sleep testing but in some cases your provider may choose a fixed pressure once the ideal settings are known. Bi-level PAP is used by some health care providers to improve comfort over standard CPAP but most of the studies do not show benefit to this approach. Bi-level can also be used for patients who do not breathe enough (hypoventilation) but is generally not needed for usual OSA.
Authors: Pamela DeYoung, RPSGT, Atul Malhotra, MD
Reviewers: Marianna Sockrider MD, DrPH, Iris Perez, MD, Helena Schotland, MD
Resources:
AMERICAN THORACIC SOCIETY – what is obstructive sleep apnea in adults?
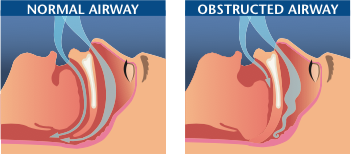 Obstructive sleep apnea (OSA) is a common problem that affects a person’s breathing during sleep. A person with OSA has times during sleep in which air cannot flow normally into the lungs. The block in airflow (obstruction) is usually caused by the collapse of the soft tissues in the back of the throat (upper airway) and tongue during sleep.
Obstructive sleep apnea (OSA) is a common problem that affects a person’s breathing during sleep. A person with OSA has times during sleep in which air cannot flow normally into the lungs. The block in airflow (obstruction) is usually caused by the collapse of the soft tissues in the back of the throat (upper airway) and tongue during sleep.
Apnea means not breathing. In OSA, you may stop breathing for short periods of time. Even when you are trying to breathe, there may be little or no airflow into the lungs. These pauses in airflow (obstructive apneas) can occur off and on during sleep, and cause you to wake up from a sound sleep. Frequent apneas can cause many problems. With time, if not treated, serious health problems may develop.
 OSA is more common in men, women after menopause and people who are over the age of 65. OSA can also occur in children. There are several groups of people who are particularly at risk for developing OSA. People who are overweight are more likely to develop sleep apnea. OSA can occur in people who have large tonsils or adenoids. OSA can also run in families of people of normal size and in people with certain types of jaw problems. People with these jaw problems have difficulty keeping the back of their throat open. Some of these conditions are called micrognathia (a small jaw) and retrognathia (a pulled back jaw).
OSA is more common in men, women after menopause and people who are over the age of 65. OSA can also occur in children. There are several groups of people who are particularly at risk for developing OSA. People who are overweight are more likely to develop sleep apnea. OSA can occur in people who have large tonsils or adenoids. OSA can also run in families of people of normal size and in people with certain types of jaw problems. People with these jaw problems have difficulty keeping the back of their throat open. Some of these conditions are called micrognathia (a small jaw) and retrognathia (a pulled back jaw).
What are the symptoms of obstructive sleep apnea?
There are many clues that tell your provider that you may have OSA. You may not be aware that you have OSA, but these symptoms may be more obvious to a spouse, other family member, or close friend.
Common symptoms you may have during sleep:
- Snoring that is usually loud and bothers other people trying to sleep near you. Snoring can come and go through the night.
- Gasping or choking sounds.
- Breathing pauses observed by someone watching you sleep.
- Sudden or jerky body movements.
- Restless tossing and turning.
- Frequent awakenings from sleep.
- Common symptoms you may have while awake.
- Wake up feeling like you have not had enough sleep, even after sleeping many hours.
- Morning headache.
- Dry or sore throat in the morning from breathing through your mouth during sleep.
- Sleepiness during the day.
- Fatigue or tiredness through the day.
- Personality changes, such as mood swings and difficulty getting along with others.
- Problems with poor memory or inability to concentrate.
Can OSA be dangerous?
Lack of sleep can cause you to fall asleep while driving and result in car accidents. Periods of stopping breathing can, with time, cause high blood pressure (hypertension), heart disease, stroke or early death.
How do I know I have OSA?
The signs of OSA described above should make you seek help for an evaluation. Discuss your problems with your health care provider. They can sort through some of the problems you are having and determine whether you should be evaluated further at a sleep center.
OSA is diagnosed by a sleep study (or polysomnogram). A sleep study is generally done at a sleep center where you will be scheduled to sleep overnight. During this time, your breathing, heart rate, sleep state and oxygen levels will be monitored.
How is obstructive sleep apnea treated?
Sleep apnea can be effectively treated, and there are a number of ways to do so. The type of treatment recommended will depend on the reason for and severity of the sleep apnea. If your OSA is from being overweight, weight loss may cause the apnea to go away completely. You can avoid alcohol for at least 4 hours before going to bed. If you sleep on your back, you can use a pillow or some other strategy to force yourself to sleep on your side. Some people sew a tennis ball into their pajama bottoms to remind them not to turn on their back.
Continuous Positive Airway Pressure (CPAP) is a common device ordered to treat most conditions of OSA. CPAP is delivered by a compressor that blows air (with or without oxygen) into a mask that is worn snugly over the nose and or mouth during sleep. The flow of air acts like a splint to keep the upper airway from collapsing. This helps prevent obstruction and the apnea from occurring. The air pressure is adjusted to a setting that best controls the apnea. Often a person will also notice much less snoring when wearing CPAP.
There are devices and surgeries which can be done to treat OSA. The type of device or surgery will depend on what has cause the apnea. Some appliances or devices (called oral devices) that are worn in the mouth during sleep may keep your airway open. Most oral devices work by either bringing the jaw forward or keeping the tongue from blocking the throat. Oral appliances are most likely to help a person who has mild sleep apnea and who is not overweight. These devices are usually custom-made and fitted under the supervision of a specialized dentist or oral surgeon who works with these problems.
Surgery may be recommended in some cases. When the tonsils or adenoids are causing the throat to be blocked, a tonsillectomy may be recommended. Surgery may also be helpful for patients with jaw problems. Other surgeries for OSA either clear out the tissue from the back of the throat or reposition the tongue forward. These surgeries are not, however, as effective as CPAP to control your OSA and are usually reserved for patients who fail CPAP.
Authors: Rowley JA, McGowen C, Lareau S, Fahy B, Garvey C, Sockrider M
For more information contact the following websites:
- American Thoracic Society
- American Academy of Sleep Medicine
- American Sleep Apnea Association
- National Heart Lung and Blood Institute
AMERICAN THORACIC SOCIETY – OBSTRUCTIVE SLEEP APNEA AND heart disease
Obstructive sleep apnea (OSA) is a condition in which you stop breathing during sleep because of OBSTRUCTED AI a narrowed or closed breathing passage (airway). Adults with obstructive sleep apnea are more likely to be overweight. Common symptoms of obstructive sleep apnea include snoring, stopping breathing during sleep, frequent awakenings during the night and difficulty staying asleep throughout the night. It is also common for patients who have obstructive sleep apnea to be tired and sleepy during the day. This sleepiness can cause accidents at work, poor work performance and car crashes. Obstructive sleep apnea can also have a bad effect on your heart and your blood vessels (arteries, veins and capillaries), which is also referred to as the cardiovascular system.
What kinds of cardiovascular problems can I get with obstructive sleep apnea?
Several cardiovascular conditions can happen with untreated obstructive sleep apnea. For example, if you have obstructive sleep apnea, you are more likely to have high blood pressure (hypertension) or it may be difficult to control your blood pressure. Of people with hypertension, about 30% have obstructive sleep apnea. If you have obstructive sleep apnea, there is a 50% chance you also have hypertension.
Problems with the rhythm of your heart may occur such as atrial fibrillation (irregular heart beat) and bradycardia (slow heart rate). Patients with severe obstructive sleep apnea are four times more likely to have atrial fibrillation compared to those without the disorder. Not receiving treatment for your sleep apnea may make your atrial fibrillation difficult to control. For example, in patients who have atrial fibrillation cured with catheter ablation (a special treatment to the heart), those with untreated obstructive sleep apnea are 25% more likely to have their atrial fibrillation return.
Patients with obstructive sleep apnea are also more likely to have coronary artery disease. Coronary artery disease (also known as the hardening of the arteries) happens when the small blood vessels that supply blood and oxygen to your heart become narrow. Narrowed coronary arteries can lead to heart attacks. If you have severe obstructive sleep apnea that is untreated, you are twice as likely to develop heart attacks in the future as those without the problem. In addition, up to 70% of patients admitted to the hospital because of coronary artery disease were found to have sleep apnea. If you have heart failure, obstructive sleep apnea can make it worse. Also, people with untreated obstructive sleep apnea can develop heart failure. The chance of having obstructive sleep apnea if you have heart failure is quite high.
How does obstructive sleep apnea cause heart disease?
The reason why patients with obstructive sleep apnea develop heart disease is not exactly known. Obstructive sleep apnea causes you to have frequent pauses in your breathing; these pauses mean that you actually stop breathing and this causes you to wake up at night. When these breathing pauses happen, the oxygen level in your blood gets low. It is thought that the frequent bouts of low oxygen levels during sleep damages the blood vessels that supply the heart. Also with each one of the episodes, your body tells your heart to beat faster and your blood pressure to go up. Severe obstructive sleep apnea can also cause stress on your heart causing the heart to get enlarged. An enlarged heart can cause the heart to get less oxygen and work less efficiently.
Will treating my obstructive sleep apnea treat my heart disease?
The most common way of treating obstructive sleep apnea is with a mechanical device known as continuous positive airway pressure (CPAP). The CPAP machine blows air through a hose into a mask worn snugly over your nose or mouth. This air goes into your lungs and keeps the airway from closing during sleep. This corrects your sleep apnea, prevents your blood oxygen levels from falling during sleep and allows you to get a restful sleep. Using CPAP regularly at night as prescribed by your health care provider also helps the stress on your heart. If you have atrial fibrillation, CPAP use may control your irregular heartbeats. If you have both severe sleep apnea and hypertension, CPAP will likely help control your blood pressure.
Patients can become comfortable with the CPAP device with time. Those who wear CPAP at night often say that they are getting the best sleep that they have gotten in a long time. Some people though may have trouble getting accustomed to sleeping with the CPAP device. If you are having difficulty, speak with the sleep specialists at the clinic to get the right nasal or full-face mask and the right setting for you. There are very good reasons to try and use the CPAP every night. CPAP therapy can help you control the symptoms of your sleep apnea and prevent or control the heart-related problems associated with sleep apnea, which are often severe and life limiting.
Authors: Jeremy Weingarten, MD and Susmita Chowdhuri, MD
Reviewers: Suzanne C. Lareau RN, MS and Margaret-Ann Carno PhD, RN, CPNP
References:
AMERICAN THORACIC SOCIETY – insomnia
 Many people experience difficulty sleeping. Some people have short periods (days to a few weeks) of difficulty falling asleep or staying asleep (called acute insomnia). Others have this difficulty for a month or longer (called chronic insomnia). About 30% of Americans complain of having insomnia. Insomnia can be very disruptive to a person’s life, so understanding insomnia and what can be done to treat it can be helpful to your quality of life.
Many people experience difficulty sleeping. Some people have short periods (days to a few weeks) of difficulty falling asleep or staying asleep (called acute insomnia). Others have this difficulty for a month or longer (called chronic insomnia). About 30% of Americans complain of having insomnia. Insomnia can be very disruptive to a person’s life, so understanding insomnia and what can be done to treat it can be helpful to your quality of life.
Insomnia is a condition that describes difficulty with sleep. This condition can include difficulty falling asleep, problems staying asleep, frequently awakening at night (fragmented sleep), and/or awakening early in the morning. This trouble sleeping results in feeling unrefreshed during the day and difficulty with daytime function including completing valued daily activities.
Who develops insomnia?
When and why insomnia begins, is not always known and therefore can be difficult to understand. We know that certain groups of people have a greater risk for developing insomnia. These include those with mood conditions (such as anxiety and/or depression), women, older people and individuals with chronic medical conditions such as asthma and COPD. Your mood can affect your sleep, but improving your sleep problem can also help symptoms of anxiety and depression.
Sleep can also be affected by medications. For example, medications often taken by those with lung problems include beta agonists, prednisone and theophylline-containing medication. Any of these can cause symptoms of insomnia.
The initial cause of your sleeping difficulty however, may not be the reason why you continue to have poor quality sleep. For example, often sleep difficulty begins as a result of a sudden event (death of a friend or family member, the break-up of a relationship, increased stress at work, or losing one’s job etc.). However, in some cases, once the event has passed and the person has recovered, the insomnia continues.
Your problems sleeping can also continue because of things you have done to try and cope with your sleep problem. For example, you may drink coffee or a caffeine containing drink in the afternoon or evening to counteract the fatigue you developed from not sleeping well. The stimulation from caffeine can have its effects on you into the evening and make it difficult for you to go to sleep, or stay asleep. You may also try drinking alcohol in the evening thinking it will help you relax and fall asleep. Alcohol can in fact also keep you from having a good night’s sleep as people tend to wake up when the alcohol wears off. Another strategy you might be tempted to try in coping with insomnia is increasing your time in bed, in hopes that this approach will result in your eventually falling asleep. However, the opposite is more likely to occur. Once trouble sleeping has taken hold, it can cause you to have negative thoughts, which can damage your confidence in your ability to sleep. Thus, a vicious cycle can develop of poor sleep, leading to anxiety about sleep, leading to a further worsening of sleep quality.
How is insomnia treated?
The first step in deciding what treatment you need is to be evaluated for the underlying cause of your insomnia, to be certain your insomnia is not from a medical condition or medications you are taking. There are some simple things you can do to help correct your insomnia. You must be patient with yourself however, as the positive effects of these treatments may not be noticeable for several days or weeks. These treatments include spending less time in bed and avoiding wake-promoting activities in bed. A sleep specialist can help guide you in making some simple changes in the hours you sleep to get you back to a normal sleep pattern. The use of a sleep log can help you keep track of your sleep.
Other things you can do are to avoid the following:
- Viewing the alarm clock.
- Exercising close to bedtime.
- Smoking cigarettes or using nicotine products (including e-cigarettes).
- Napping and irregular bedtimes.
- Eating heavy meals close to bedtime.
- Drinking a lot of fluid late at night.
Once these are not found to be the source of your problem, your health care provider may recommend a brief course of sleeping pills (medication) to help you break the cycle of insomnia or suggest behavioral modification treatment. Behavioral modification can be just as helpful and have longer lasting effects than medication without risk of adverse side effects.
Expect that you may feel tired following a poor night’s sleep. This discomfort will only be for a short time. Accepting your sleeplessness will help you avoid extreme negative thoughts regarding sleep.
Can over the counter medications help me sleep?
Some over-the-counter medication (not needing a prescription) may be helpful, but many of these drugs have not had enough study for your health care provider to feel they are safe or will help you. Check with your health care provider to make sure that any over-the-counter medications you are taking don’t interfere with your other medications. Unless you suffer from a condition requiring pain treatment or a fever reducer, you should avoid over-the-counter sleep aids that contain additional pain medication, such as acetaminophen.
Is insomnia a serious health problem?
Insomnia can be serious and a sign of more serious sleep problems such as sleep apnea that affect your lungs and heart. Sleepiness during your waking hours will make you an unsafe driver. Accidents happen during the day as well as at night from people who are sleep deprived.
Conditions that mimic (act like) insomnia.
Some individuals complain not of difficulty sleeping, but of wanting to sleep at the “wrong” times. These are usually from circadian rhythm (body clock) problems. They may fall asleep late and wake up late, this condition is referred to as Delayed Sleep Phase Syndrome. Or they may fall asleep too early in the evening and wake up in the early morning, this condition is called Advanced Sleep Phase Syndrome. If you have either of these problems, bright light therapy or melatonin may be recommended. However, these treatments need to be given at a specific time in your sleep/wake cycle in order to be helpful in correcting your sleep problem. Discuss with your provider since the details of the timing are important.
By changing a few things related to your sleep, you can dramatically improve your sleep quality. Try not to become discouraged if your sleep doesn’t improve immediately.
If you have tried all of these suggestions regularly for several weeks without benefit or have serious concerns about your insomnia, get professional help. For help with your sleep difficulty, you can find a list of sleep specialists SleepEducation.com or ask your health care provider for a referral.
Authors: Matthew R. Ebben PhD, D,ABSM, CBSM, FAASM and Mary C. Kapella PhD, RN
Reviewers: Atul Malhotra MD, Suzanne C Lareau RN, MS and Marianna Sockrider, MD, DrPH
Resources:
